Collaboration with Children’s National Hospital aims to reduce child mortality rates caused by Sickle Cell kidney failure
Katarina Benson
Children with Sickle Cell Disease (SCD), a genetic disorder affecting red blood cells, experience terrible bouts of pain when the blood cells contort into a sickle shape and block small blood vessels, hindering oxygen delivery to critical organs. Whenever these bouts occur in the kidneys, the filtration system of the kidneys can be irreversibly damaged. Kidney failure is associated with a 30% death rate in SCD patients.
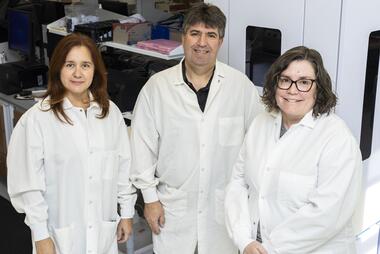
In partnership with Children’s National Hospital, scientists at George Mason University have discovered a new way to detect early signs of kidney damage in childhood patients with SCD. A recently awarded two-year $200,000 grant from the Commonwealth Health Research Board will support a team led by George Mason systems biologist and research fellow Marissa Howard; Children’s National Comprehensive Sickle Cell Disease Program Director Andrew Campbell, MD; and urinary biomarker expert Oliver John Semmes, of Old Dominion University.

The multi-institutional trial leverages unique proteomic expertise blended within the Children’s National SCD Program’s ongoing clinical study of the progress of SCD within pediatric patients over time and will transform kidney disease detection in these SCD patients.
According to the Sickle Cell Disease Association of America, SCD is a global health problem that affects an estimated 100,000 people in the United States, with about 2,000 babies annually being diagnosed with the disease at birth. With each SCD crisis, kidney damage accumulates, increasing the risk of total kidney failure mortality for SCD patients. Early detection of kidney damage, especially in childhood, allows for rapid treatment and prevention of long-term kidney damage-related effects.
“Our team will analyze the actual damaged mitochondria, the power houses of the cell, that are crippled by lack of oxygen that occurs during each sickle-cell crisis,” said Howard, who first reported this pathway and methodology to rescue mitochondrially damaged cells in her prior National Institutes of Health-supported and published research.
“We measure these damaged mitochondria shed by the kidney in a few milliliters of urine so we can develop an early warning system for the onset of kidney damage,” said Howard, an expert in isolation of extracellular vesicles (EVs), small packages of cellular information shed into the urine, and the methods required to complete this analysis. “Our partners at Children’s National are known for identifying innovative approaches to treat SCD. This exciting collaboration is collectively motivated by our ultimate goal of reducing the high mortality rate caused by Sickle Cell kidney failure in children affected by this disease.”
Children’s National Comprehensive Sickle Cell Disease Program, among the largest in the country, follows more than 1,500 patients from birth through age 21 and is one of the few centers offering gene therapy treatments for SCD. The program has amassed a large base of patient samples, some of which will be analyzed in this project.
Campbell, a physician-scientist caring for SCD patients at Children’s National, will oversee the recruitment, consenting, and collection of biological samples throughout the study’s duration, as well as coordinate the delivery of these samples to George Mason’s CAP/CLIA certified laboratory facilities for analysis.
While current screening methods rely on established urine tests for albumin, this groundbreaking research will use advanced proteomic analysis to detect kidney injury at its earliest stages—before conventional tests show abnormalities.
“We’ve watched as silent kidney damage progresses year after year, often going undetected until significant harm has occurred,” said Campbell. “By identifying kidney disease earlier, we can intervene sooner with more effective disease-modifying therapies and curative treatments, potentially preventing or slowing progression to kidney failure.”
According to Campbell, this grant is more than funding—it’s a commitment to SCD patients and their families, a collaboration to build the next generation of diagnostics, which can fundamentally change how to manage SCD and protect the health of children and young adults living with this debilitating disease.
“This partnership leverages our collective strengths to address a compelling global challenge that might have a multitude of applications,” shared Lance Liotta, MD, codirector of George Mason’s Center for Proteomics and Molecular Medicine (CAPMM), who will certify that all work performed is under CAP/CLIA compliance for the data to be presented to the FDA for future clinical application.
George Mason is highly regarded for offering real world, hands-on learning experiences for its science students, and this medical research project is no exception. As part of George Mason’s Office of Student Creative Activities and Research Undergraduate Research Scholars Program, Naureen Zahra, who had interned the previous summer at the National Institutes of Health on a project focused on curing SCD with bone marrow transplants, performed portions of this experimental study over the summer.

“One of my educational goals was to become an expert in performing key molecular biology techniques such as western blots to analyze the presence of proteins like PINK1, which plays a key role in regulating mitochondrial health,” said Zahra, a neuroscience major. The team worked to isolate EVs from Children’s National patient urine samples and analyze protein data. “Working with these scientists on actual patient samples connected me to real-world outcomes, expanding my sense of empathy for what these children are going through.”
In addition to its potential to improve the lives of those affected by SCD, this research effort may also have even wider impact.
“These findings could also serve as a new marker for mitochondrial damage for a variety of diseases including Parkinson’s, heart disease, and diabetic kidney disease,” said Howard. “In addition, urinary biomarkers could offer a predictive tool to guide SCD therapy management and therapy effectiveness more holistically.”