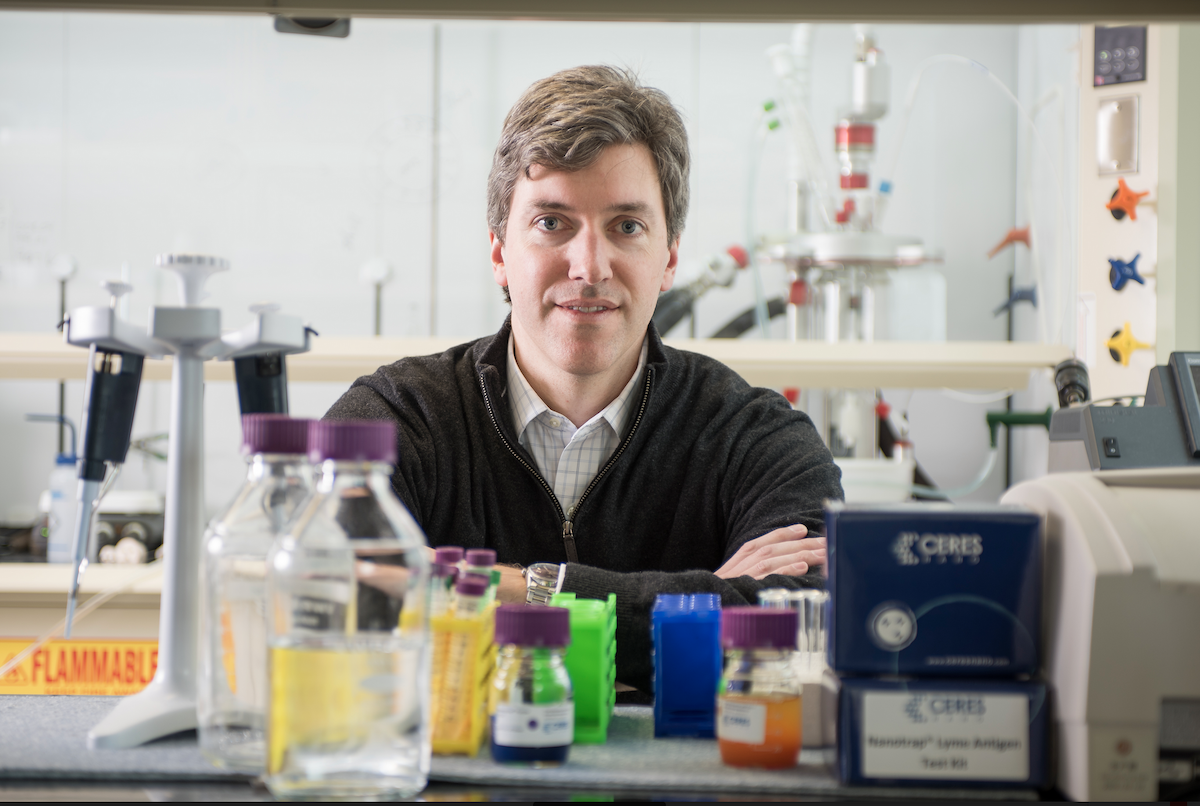
Study the latest innovations in personalized medicine that have transformed prevention, diagnosis, and treatment. International experts provide examples of exciting laboratory discoveries and translate them to patient bedsides.
New Summer Break Study Abroad Program Translational Medicine: From Bench to Bedside to The Community. See flyer for details below.
Italy-Translational-Medicine-From-Bench-to-Bedside-to-the-Community