It isn’t often that someone graduates with a PhD and a scientific discovery, but George Mason University researcher Marissa Howard was no ordinary student.
Marissa Howard
Howard, BS Bioengineering ’17, PhD Biosciences ’22, leads a team of scientists who have discovered a way to “eavesdrop” on cellular communications that could revolutionize treatments for cancer and other maladies.
All cells are constantly communicating with other cells using what Howard calls “an internet of molecular information.” Researchers at Mason’s Center for Applied Proteomics and Molecular Medicine (CAPMM), where Howard has worked since she was an undergraduate, are the first scientists to successfully tap into this communications system, which tumors use to trick or block the immune system and attract normal cells.
Howard was recently awarded a $200k grant from the National Cancer Institute to further this work. It is a medical breakthrough that could drastically change the way cancer is treated.
“It’s fun to be able to get to the source of tumors and actually figure out what’s going on there,” said Howard, who completed some of this work as part of her dissertation. “That’s what all cancer researchers want to do—figure out what the tumor is ‘thinking’ so we can get better outcomes for patients.”
Howard and the team have been focused on a component of the cellular communication system called extracellular vesicles (EVs), which are packages of concentrated information housed within tiny membrane-enclosed bubbles. The EVs are shed from the surface of cells and can travel long distances to be received by distant cells, causing a change in the behavior of the message recipient.
In the past, EVs were studied in cultured cells or were captured from a patient’s blood, but the Mason team created a way to study the cancer EVs within a solid living tumor at their source by sampling the interstitial fluid (IF), the wet environment that bathes all cells within tissues. This is the first portrait of the tumor EV communication system at its origin. Their findings, with Howard as first author, were published in the Journal of Extracellular Vesicles.
Their research also showed a dramatic difference in the communication function of the different major types of tumor tissue EVs. The scientists isolated the two major types of tumor EVs and then used nanoparticles, a Nanotrap technology created by CAPMM researchers, to deliver them to a draining lymph node.
Howard said that the treatment of the lymph node with the two separate classes of EVs was associated with dramatic differences in the growth of distance metastasis in the lung. “Repeated tests done in mice proved one class of isolated mitochondrial EVs capable of preventing the metastasizing of cancerous breast tumors while another class promoted cancerous growth.”
The discovery means doctors could more quickly gauge the effectiveness of existing cancer treatments and make real-time adjustments based on the information derived from the cellular communications.
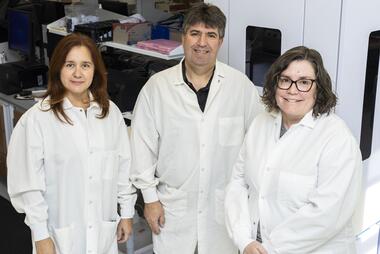
Marissa Howard with CAPMM Director Lance Liotta and College of Science Dean Fernando Miralles at Mason Innovation Awards. Photo by John Boal Photography
It’s for that reason that the team’s discoveries have further implications beyond cancer, according to Lance Liotta, a Distinguished University Professor at Mason and the cofounder and codirector of CAPMM.
“These specific markers for mitochondrial health allow EVs to be a novel biomarker/diagnostic tool for cancer and other mitochondrial disorder diseases, such as Parkinson’s disease, Alzheimer’s, Lou Gehrig’s disease, or muscular dystrophy,” Liotta said.
Howard first began working with Liotta and other CAPMM scientists as a bioengineering major participating in Mason’s Aspiring Scientists Summer Internship Program, where she spent the summer studying the electrical properties of their Nanotrap technology.
“I really loved it,” she said of the work. “[The CAPMM scientists] were excited by the work I was doing and asked me to continue working with them. I’ve been in the CAPMM lab since 2016.”
Howard is also an inventor and shares several patents with her CAPMM colleagues. For her senior capstone project, Howard led a team of bioengineering students to create a noninvasive urine-based tuberculosis (TB) test using CAPMM’s Nanotrap technology, and the invention, called TB Assured, garnered a lot of attention for the team and many awards, including a $15,000 prize from the National Institute of Biomedical Imaging and Bioengineering’s Design by Biomedical Undergraduate Teams (DEBUT) challenge to help develop the test further.
“Everything that’s in the urine is captured by the Nanotraps, and you don’t need a centrifuge or other equipment,” said Howard, who completed her bachelor’s degree in bioengineering in 2017. “People loved it. They keep asking when it is going to be available at their local pharmacy.”
“I love the research space and the creative potential that comes with it,” Howard said. “You never know when your next idea is going to pop up.”
In addition to Howard and CAPMM’s Liotta, the EV research collaboration also included Alessandra Luchini, Amanda Haymond, and Fatah Kashanchi within the College of Science; collaborator Robyn Araujo at Queensland University in Australia; graduate students James Erickson, Zachary Cuba, Weidong Zhou, Purva Gade, Rachel Carter, Kelsey Mitchell, Heather Branscome, Fatimah Alanazi, Yuriy Kim; and high school students Shawn Kim and Daivik Siddhi.
Colleen Kearney Rich contributed to this article.